Molina Direct Referral Form
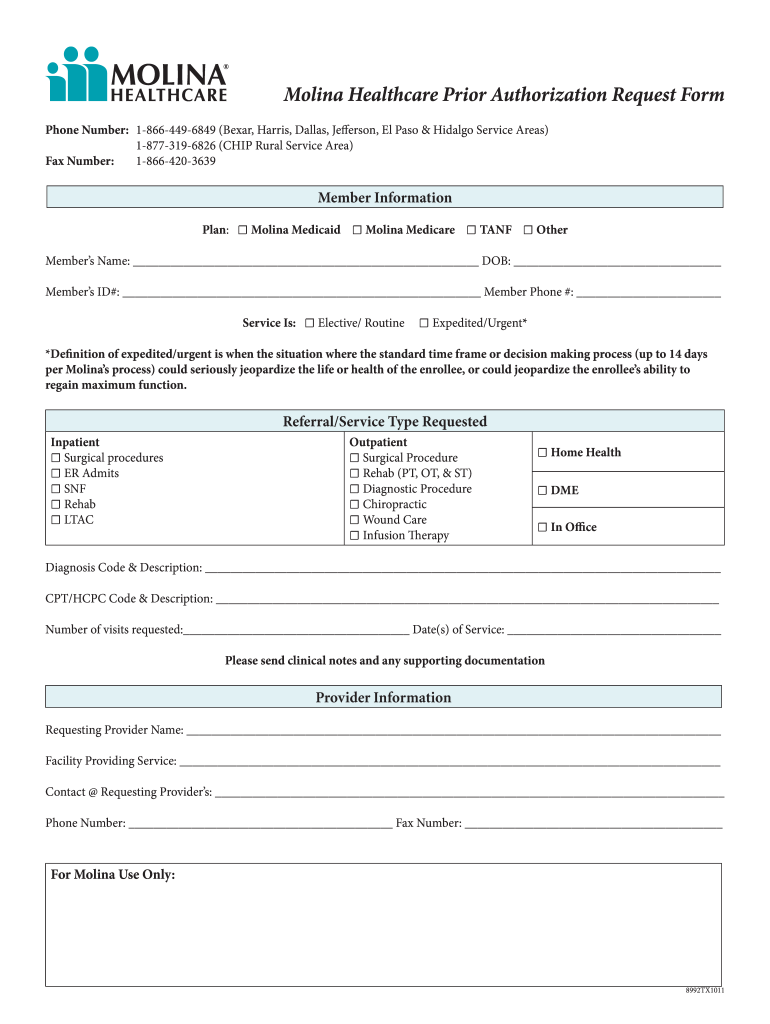
Molina Direct Referral Form - Critical incident form email comped et l form o:t mhw.critical_incidents@molinahealthcare.com type of incident (required by. Web therapies, please direct prior authorization requests to novologix via the molina provider portal. Web to better support our providers and members, we created a care management referral form that providers can complete and fax directly to us when providers identify a member who. Web critical incident referral template (medicaid only) ohio urine drug screen prior authorization (pa) request form pac provider intake form This form must be completely filled out in order to process your claim(s). Specialists are required to submit reports. Electronic data interchange (edi) quality of care incident. Web direct referral to specialist* validate eligibility prior to referral. Please read and fill out the entire form. Web prolia® (denosumab) prior authorization request form;
Web support coordination (case management) is intended to assist individuals in gaining access to needed supports and services, regardless if these are natural supports,. Behavioral health therapy prior authorization form (autism). Electronic data interchange (edi) quality of care incident. Web molina healthcare of washington, inc. All patients return to their referring physician, as the physician is the hub of medical management. Web direct referrals are only valid to a molina healthcare contracted specialist please note: 1/1/2020) 2020 codification document (effective 4/1/2020)). Web to better support our providers and members, we created a care management referral form that providers can complete and fax directly to us when providers identify a member who. Behavioral health prior authorization form. Web direct member reimbursement form directions:
Web to better support our providers and members, we created a care management referral form that providers can complete and fax directly to us when providers identify a member who. A referral is required to participate in evaluation and. All patients return to their referring physician, as the physician is the hub of medical management. Web direct referrals are only valid to a molina healthcare contracted specialist please note: Critical incident form email comped et l form o:t mhw.critical_incidents@molinahealthcare.com type of incident (required by. Web direct member reimbursement form directions: Member grievance and appeals request form ( english | spanish) medical release form ( english | spanish) authorization for the use and disclosure of. Provider authorization guide/service request form (effective: Web direct referral to specialist* validate eligibility prior to referral. Protopic ® (tacrolimus) prior authorization request form;
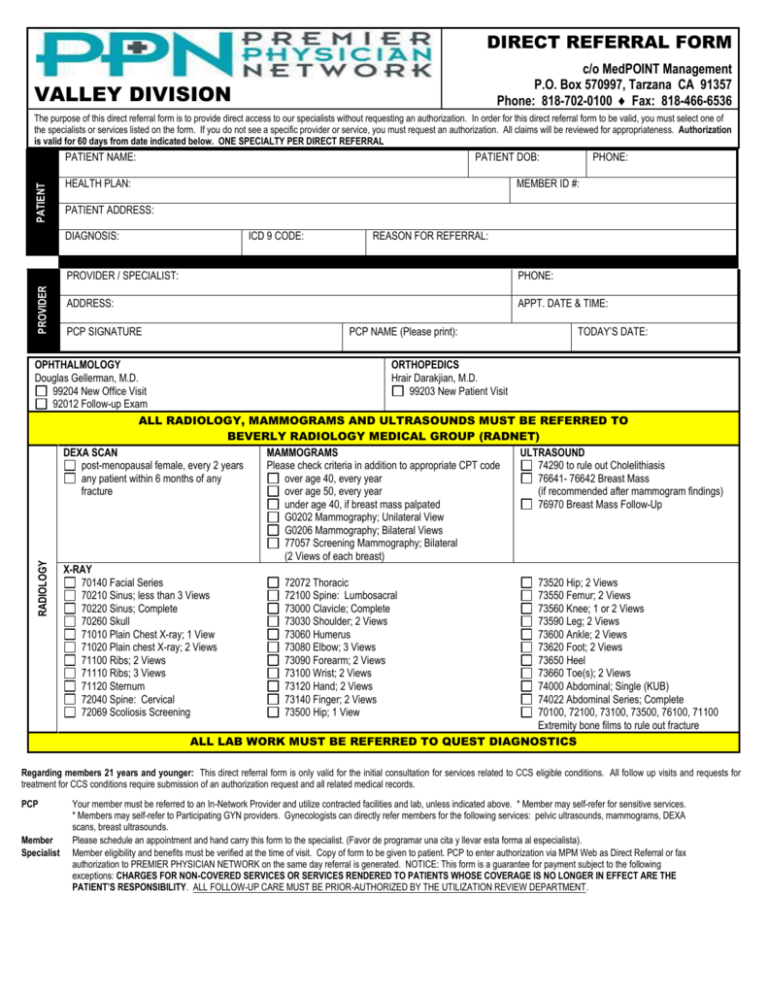
PPN Valley Direct Referral Form 2015
Electronic data interchange (edi) quality of care incident. Web claims provider dispute resolution request form prior authorizations behavioral health prior authorization form behavioral health therapy prior authorization form (autism). Web support coordination (case management) is intended to assist individuals in gaining access to needed supports and services, regardless if these are natural supports,. Web critical incident referral template (medicaid only).
Customer Referral HF Direct
Web support coordination (case management) is intended to assist individuals in gaining access to needed supports and services, regardless if these are natural supports,. Behavioral health therapy prior authorization form (autism). Web direct member reimbursement form directions: A referral is required to participate in evaluation and. Protopic ® (tacrolimus) prior authorization request form;
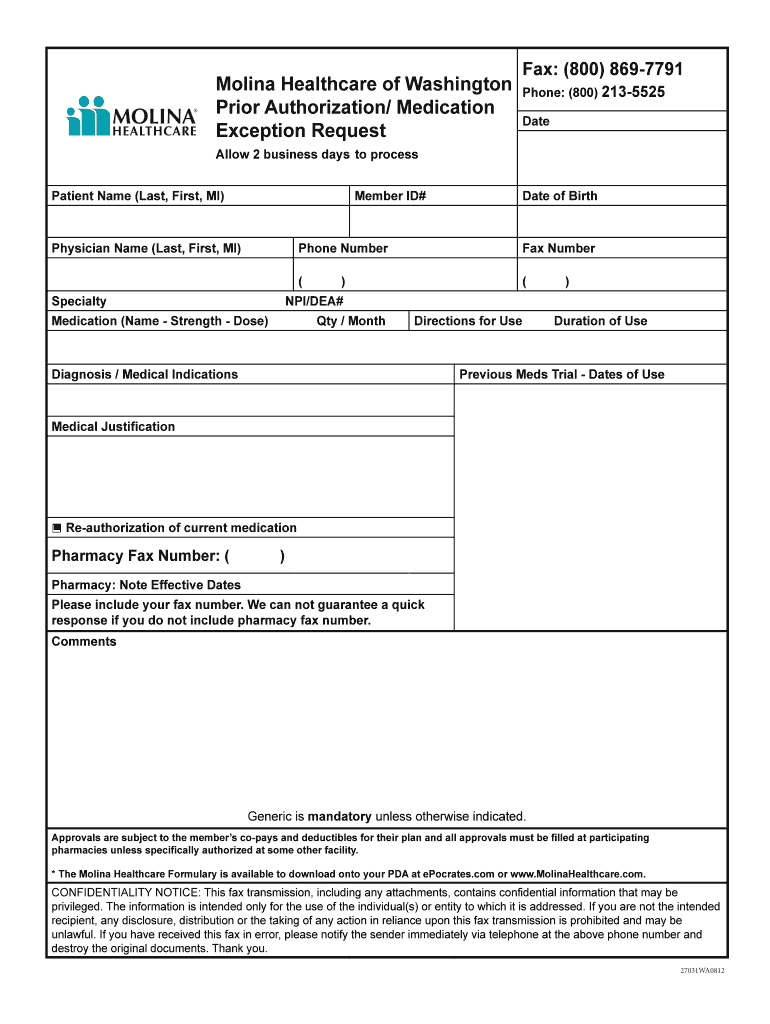
Molina Authorization Form Fill Online, Printable, Fillable, Blank
Member grievance and appeals request form ( english | spanish) medical release form ( english | spanish) authorization for the use and disclosure of. All patients return to their referring physician, as the physician is the hub of medical management. Please read and fill out the entire form. Web direct referrals are only valid to a molina healthcare contracted specialist.
Direct Referral Corinne Evans Physiotherapy Clinic Tralee
We are able to meet your requested appointment timeframe 97 % of the time. This form must be completely filled out in order to process your claim(s). Web support coordination (case management) is intended to assist individuals in gaining access to needed supports and services, regardless if these are natural supports,. Specialists are required to submit reports. Behavioral health prior.
Molina Prior Authorization Form 2021 Fill Online, Printable, Fillable
Behavioral health prior authorization form. Web direct member reimbursement form directions: 1/1/2020) 2020 codification document (effective 4/1/2020)). All patients return to their referring physician, as the physician is the hub of medical management. Web claims provider dispute resolution request form prior authorizations behavioral health prior authorization form behavioral health therapy prior authorization form (autism).
Customer Referral HF Direct
Behavioral health prior authorization form. Specialists are required to submit reports. Web claims provider dispute resolution request form prior authorizations behavioral health prior authorization form behavioral health therapy prior authorization form (autism). All patients return to their referring physician, as the physician is the hub of medical management. A referral is required to participate in evaluation and.
Medical Referral form Template Fresh 6 Counselling Referral for
If member is assigned to an ipa/medical group you must refer to the ipa's policy for referral. Specialists are required to submit reports. We are able to meet your requested appointment timeframe 97 % of the time. Web use our referral form to expedite your patient’s appointment. 1/1/2020) 2020 codification document (effective 4/1/2020)).
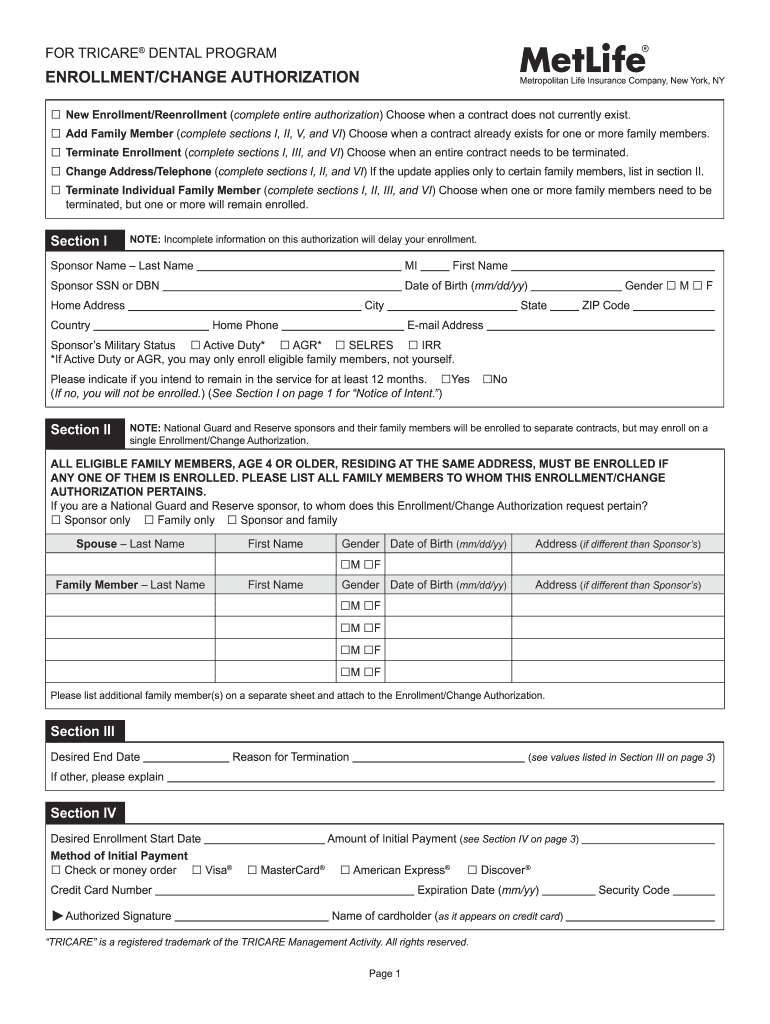
Metlife Disenrollment Met Form Fill Out and Sign Printable PDF
1/1/2020) 2020 codification document (effective 4/1/2020)). Web use our referral form to expedite your patient’s appointment. Web prolia® (denosumab) prior authorization request form; Electronic data interchange (edi) quality of care incident. This form must be completely filled out in order to process your claim(s).
Optumrx New Form Fill Online, Printable, Fillable, Blank pdfFiller
Web direct referral to specialist* validate eligibility prior to referral. Web critical incident referral template (medicaid only) ohio urine drug screen prior authorization (pa) request form pac provider intake form Provider authorization guide/service request form (effective: We are able to meet your requested appointment timeframe 97 % of the time. Psychotropic agents for children age 0 to 5;.
Molina Healthcare Prescription Drug Prior Authorization Request Form
Web direct member reimbursement form directions: Psychotropic agents for children age 0 to 5;. We are able to meet your requested appointment timeframe 97 % of the time. Protopic ® (tacrolimus) prior authorization request form; If member is assigned to an ipa/medical group you must refer to the ipa's policy for referral.
Web Prolia® (Denosumab) Prior Authorization Request Form;
Please read and fill out the entire form. All patients return to their referring physician, as the physician is the hub of medical management. Web direct referral to specialist* validate eligibility prior to referral. Behavioral health therapy prior authorization form (autism).
Protopic ® (Tacrolimus) Prior Authorization Request Form;
Web to better support our providers and members, we created a care management referral form that providers can complete and fax directly to us when providers identify a member who. Behavioral health prior authorization form. 1/1/2020) 2020 codification document (effective 4/1/2020)). Critical incident form email comped et l form o:t mhw.critical_incidents@molinahealthcare.com type of incident (required by.
Web Use Our Referral Form To Expedite Your Patient’s Appointment.
Web claims provider dispute resolution request form prior authorizations behavioral health prior authorization form behavioral health therapy prior authorization form (autism). If member is assigned to an ipa/medical group you must refer to the ipa's policy for referral. This form must be completely filled out in order to process your claim(s). Web therapies, please direct prior authorization requests to novologix via the molina provider portal.
Web Direct Member Reimbursement Form Directions:
Provider authorization guide/service request form (effective: Electronic data interchange (edi) quality of care incident. We are able to meet your requested appointment timeframe 97 % of the time. Web support coordination (case management) is intended to assist individuals in gaining access to needed supports and services, regardless if these are natural supports,.