Molina Complete Care Prior Authorization Form
Molina Complete Care Prior Authorization Form - Only covered services are eligible for reimbursement. Molina healthcare of mississippi , inc. Member information member’s last name: Web pharmacy prior authorization forms. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Web updated july 27, 2023. Our holistic approach to specialty benefit management consistently drives over 7% immediate savings, 50% ongoing trend reduction and the highest levels of quality and physician satisfaction. • prescriber first name, last name, npi, phone number and fax. Please refer to molina complete care (mcc)’s provider website or prior authorization (pa) lookup tool for specific codes that require authorization. Care (310) ☐ outpatient bh behavioral health (230), behavioral health intermediate.
Web prior authorization requests. Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. Please refer to molina complete care (mcc)’s provider website or prior authorization (pa) lookup tool for specific codes that require authorization. Please use one form per member. Care (310) ☐ outpatient bh behavioral health (230), behavioral health intermediate. Our holistic approach to specialty benefit management consistently drives over 7% immediate savings, 50% ongoing trend reduction and the highest levels of quality and physician satisfaction. Member information member’s last name: It is needed before you can get certain services or drugs. Web molina complete care prior authorization (pa) form prescription drug if the following information is not complete, correct, or legible, the pa process can be delayed. Pharmacy prior authorization contacts (coming soon) molina complete care.
It should be noted that the medical office will need to provide justification for requesting the specific medication, and that authorization is not guaranteed. Web members > medicaid > about medicaid > getting care > prior authorizations prior authorizations what are prior authorizations? Molina healthcare of iowa will only process completed pa request forms, the following information must be included for the request form to be considered complete: Pharmacy prior authorization contacts (coming soon) molina complete care. Pharmacy prior authorization forms ; Managing the cost of specialty care doesn’t require abrasive physician oversight. It is needed before you can get certain services or drugs. 01/01/2022 refer to molina’s provider website or prior authorization look up tool/matrix for specific codes that require authorization only covered services are eligible for reimbursement Request for psychological and neuropsychological testing preauthorization form My health pays rewards® ways to save;
Molina Drug Prior Authorization Fill Online, Printable, Fillable
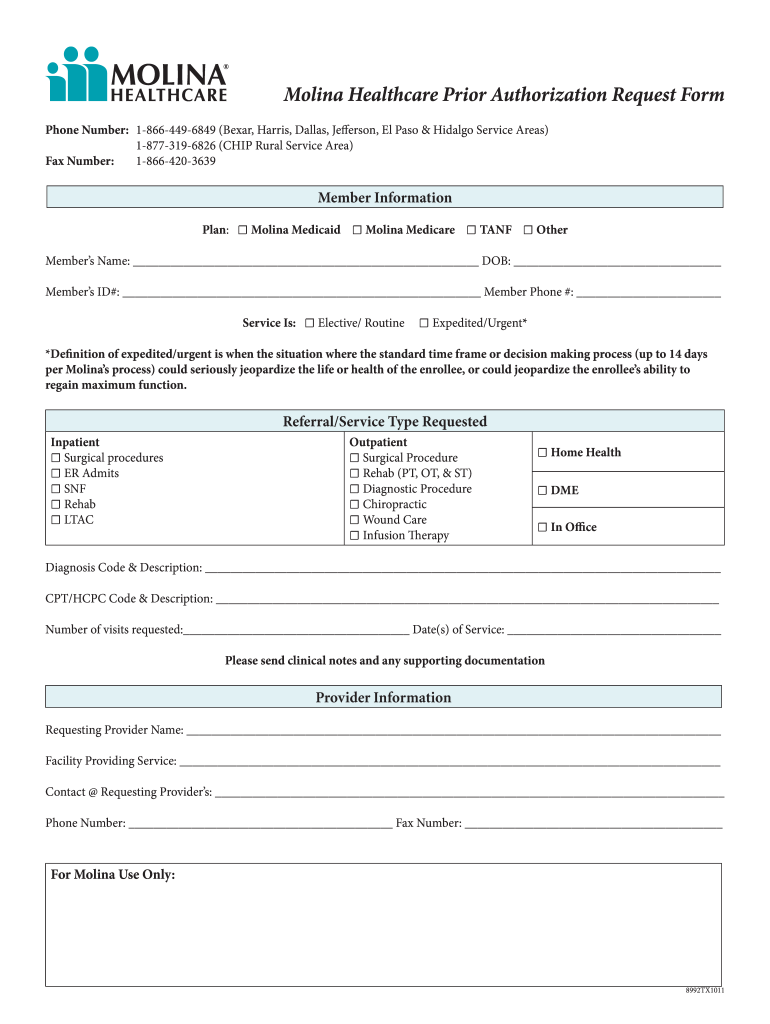
My health pays rewards® ways to save; Request for psychological and neuropsychological testing preauthorization form Please use one form per member. The fastest route for prior authorization is submission via fax. Molina healthcare prior authorization request form and instructions.
Prior Form Florida Fill Online, Printable, Fillable, Blank pdfFiller
Please use one form per member. Web home our health plans show our health plans menu about our plans; • member first name, last name, date of birth and identification number. We have provided all of the necessary. Molina healthcare prior authorization request form and instructions.
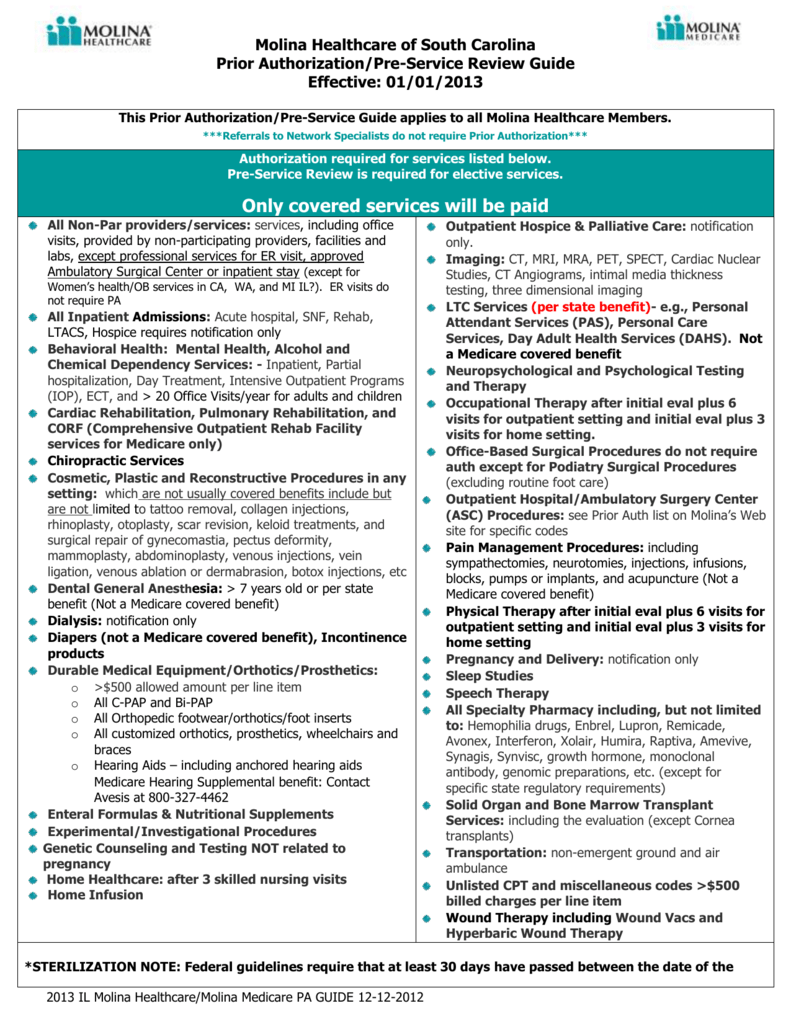
Prior Authorization/PreService Review Guide
2019 medicaid pa guide/request form effective 07.01.20 Molina healthcare of iowa will only process completed pa request forms, the following information must be included for the request form to be considered complete: Web pharmacy prior authorization forms. Care (310) ☐ outpatient bh behavioral health (230), behavioral health intermediate. • prescriber first name, last name, npi, phone number and fax.
Molina prior authorization form Fill out & sign online DocHub
2019 medicaid pa guide/request form effective 07.01.20 Web submitting a prior authorization request. A molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s prescription. Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. The fastest route for prior authorization is.
Standard Pharmacy Prior Authorization Form for Prepaid Health Plans
• prescriber first name, last name, npi, phone number and fax. The fastest route for prior authorization is submission via fax. Web molina complete care prior authorization (pa) form prescription drug if the following information is not complete, correct, or legible, the pa process can be delayed. 01/01/2022 refer to molina’s provider website or prior authorization look up tool/matrix for.
Aarp Medicare Supplement Prior Authorization Form Form Resume
Web home our health plans show our health plans menu about our plans; We have provided all of the necessary. Molina healthcare prior authorization request form and instructions. It is needed before you can get certain services or drugs. Please refer to molina complete care (mcc)’s provider website or prior authorization (pa) lookup tool for specific codes that require authorization.
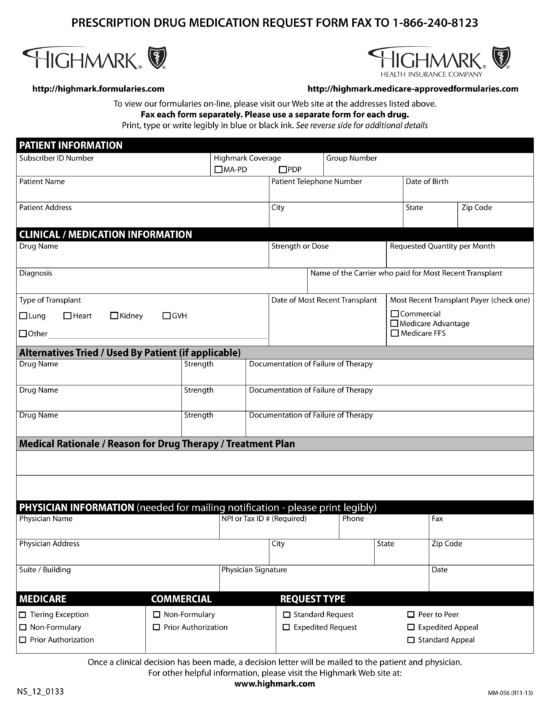
Free Highmark Prior (Rx) Authorization Form PDF eForms
Web home our health plans show our health plans menu about our plans; Web refer to molina’s provider website or portal for specific codes that require authorization. Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. My health pays rewards® ways to save; • prescriber first name,.
Fill Free fillable Mercy Care PDF forms
Web home our health plans show our health plans menu about our plans; Please use the “find a provider” tool above, which features pdf versions of our provider directories. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Member information member’s last name: Molina healthcare contact information prior authorizations:
Molina Healthcare Molina Medicare Prior Authorization Request form
2019 medicaid pa guide/request form effective 07.01.20 Molina healthcare contact information prior authorizations: Pharmacy prior authorization forms ; • member first name, last name, date of birth and identification number. Request for psychological and neuropsychological testing preauthorization form
WA Molina Healthcare Behavioral Health Authorization/Notification Form
Web submitting a prior authorization request. Web home our health plans show our health plans menu about our plans; 2019 medicaid pa guide/request form effective 07.01.20 Pharmacy prior authorization contacts (coming soon) molina complete care. Member information member’s last name:
Prior Authorization Is When Your Provider Gets Approval From Molina Healthcare To Provide You A Service.
It is needed before you can get certain services or drugs. Only covered services are eligible for reimbursement. Please use one form per member. Please use the “find a provider” tool above, which features pdf versions of our provider directories.
Our Holistic Approach To Specialty Benefit Management Consistently Drives Over 7% Immediate Savings, 50% Ongoing Trend Reduction And The Highest Levels Of Quality And Physician Satisfaction.
Web pharmacy prior authorization forms. The fastest route for prior authorization is submission via fax. Web prior authorization requests. Web refer to molina’s provider website or portal for specific codes that require authorization.
Member Information Member’s Last Name:
Please refer to molina complete care (mcc)’s provider website or prior authorization (pa) lookup tool for specific codes that require authorization. Molina healthcare contact information prior authorizations: Web effective march 3, 2022 services listed below require prior authorization. Care (310) ☐ outpatient bh behavioral health (230), behavioral health intermediate.
Web The Molina Healthcare Of Ohio Preferred Drug List (Pdl) Was Created To Help Manage The Quality Of Our Members’ Pharmacy Benefit.
Pharmacy prior authorization contacts (coming soon) molina complete care. • member first name, last name, date of birth and identification number. We have provided all of the necessary. Web updated july 27, 2023.